Imagine a healthcare system where claims are processed with lightning speed, errors are virtually eliminated, and fraudulent activities are detected before they can cause significant financial damage. This vision is no longer a distant aspiration but a tangible reality being crafted by Artificial Intelligence (AI) within the realm of healthcare claims management. As the healthcare sector faces mounting costs and increasingly complex processes, AI is stepping in as a transformative force, revolutionizing the intricate journey of managing medical insurance claims from initial submission to final reimbursement. By automating repetitive tasks, enhancing accuracy, and providing deep insights, AI is streamlining operations for healthcare providers and insurers alike. This article delves into the profound impact of AI on this critical industry segment, exploring how technology is addressing longstanding challenges and paving the way for a more efficient future in claims processing.
Revolutionizing Operations with Automation
The integration of AI into healthcare claims management is fundamentally altering operational workflows by automating routine and labor-intensive tasks. AI-powered tools, such as virtual assistants and chatbots, are now adept at managing real-time inquiries from both providers and patients, offering guidance through the often convoluted claims process. Simultaneously, automated systems are taking over repetitive functions like data entry and document handling, significantly reducing human error and accelerating processing timelines. This shift allows staff to redirect their focus toward more nuanced tasks that require critical thinking and expertise, thereby enhancing overall productivity. The result is a noticeable improvement in the speed of reimbursements, ensuring that healthcare providers receive payments promptly and can maintain financial stability in an industry often strained by delayed cash flows.
Beyond simply speeding up processes, AI-driven automation is also contributing to a higher standard of accuracy in claims management. By minimizing manual intervention, these systems reduce the likelihood of mistakes in coding medical procedures or verifying patient information, which historically have led to claim denials or rejections. Furthermore, automation fosters consistency across large volumes of claims, ensuring that each case is handled with the same precision, regardless of workload pressures. This reliability not only benefits healthcare providers by reducing administrative burdens but also enhances trust among insurers and patients who rely on timely and accurate processing. As AI continues to refine these automated processes, the healthcare claims landscape is becoming a model of efficiency, setting a new benchmark for operational excellence in the sector.
Combating Fraud with Intelligent Detection
One of the most critical advantages of AI in healthcare claims management lies in its ability to address the pervasive issue of fraud, which costs the industry billions of dollars each year. Advanced AI algorithms are designed to sift through enormous datasets, identifying subtle patterns or anomalies that may signal fraudulent behavior. Unlike traditional manual audits that often occur after the damage is done, AI offers a proactive approach by flagging suspicious claims in real time, allowing insurers to intervene before financial losses mount. This capability is proving invaluable in an era where fraudulent schemes are becoming increasingly sophisticated, providing a robust defense mechanism that protects both resources and the integrity of the claims process.
Moreover, the impact of AI on fraud detection extends beyond financial savings to foster greater confidence in the healthcare system as a whole. By consistently identifying and mitigating risks, these intelligent systems help build trust among stakeholders, including providers, insurers, and policyholders, who can be assured that the process is safeguarded against abuse. Additionally, the data gathered through AI analysis can inform future strategies to prevent fraud, creating a feedback loop that continuously strengthens defenses. This not only deters potential bad actors but also ensures that legitimate claims are processed without unnecessary delays caused by blanket suspicion or overzealous manual reviews. The role of AI in this domain marks a significant advancement, transforming a reactive industry into one that anticipates and neutralizes threats with precision.
Enhancing Decisions through Predictive Analytics
AI is also reshaping healthcare claims management by leveraging predictive analytics to drive smarter, more strategic decision-making. By analyzing extensive historical data, AI models can forecast the likely outcomes of claims, pinpointing those with a higher risk of denial or complication. This foresight enables insurers to allocate resources more effectively, prioritizing complex cases while expediting straightforward ones. Such an approach not only streamlines operations but also enhances customer satisfaction by reducing wait times for claim resolutions. The ability to anticipate challenges before they arise represents a paradigm shift, moving the industry away from reactive problem-solving toward a proactive, data-driven framework that optimizes every facet of the claims process.
In addition to improving operational efficiency, predictive analytics powered by AI offers substantial cost-saving opportunities for both insurers and healthcare providers. By identifying trends and potential bottlenecks early, organizations can implement targeted interventions that prevent costly delays or disputes. This analytical depth also supports better policy design, as insurers gain insights into claim patterns that can inform more equitable and effective coverage plans. For providers, the ability to predict high-risk claims means they can address documentation or coding issues upfront, avoiding the financial strain of rejections. As these tools become more sophisticated, their integration into claims management is setting a new standard for precision and foresight, ensuring that decisions are grounded in actionable intelligence rather than guesswork.
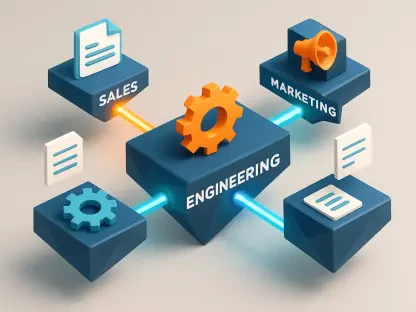
Shaping the Future with Digital Synergy
The trajectory of AI in healthcare claims management points to a broader movement toward digital transformation that promises to redefine the industry. When paired with cloud-based platforms, AI offers unparalleled scalability and accessibility, making cutting-edge tools available to organizations regardless of size or budget. This democratization of technology ensures that even smaller providers can benefit from the efficiencies that AI brings, leveling the playing field in a competitive market. Moreover, the adaptability of these systems means they can keep pace with emerging trends such as telemedicine, seamlessly managing claims for virtual care services that are becoming increasingly prevalent in today’s healthcare landscape.
Looking ahead, the synergy between AI and other digital innovations is set to unlock even greater potential for claims management. As machine learning algorithms evolve, they will refine their ability to handle complex, non-standard claims with minimal human oversight, further reducing costs and errors. Additionally, the integration of AI with blockchain technology could enhance security and transparency, creating an immutable record of claims transactions that all parties can trust. This forward momentum suggests a future where claims processing is not just efficient but also inherently resilient to the challenges of a rapidly changing healthcare environment. With AI leading the charge, the industry is on the cusp of a transformation that prioritizes innovation, benefiting providers, insurers, and patients in equal measure.