In an age where fraudsters constantly evolve their tactics, Medicare beneficiaries have a key tool at their disposal to combat health care fraud: the Medicare Summary Notice (MSN). Each MSN provides a detailed record of services and supplies billed to Medicare, effectively serving as a valuable personal fraud prevention system. As health care fraud continues to drain billions of dollars from the Medicare program annually, understanding and leveraging the information within these statements are crucial steps in protecting oneself and the overall integrity of the Medicare system.
Understanding Your Medicare Summary Notices
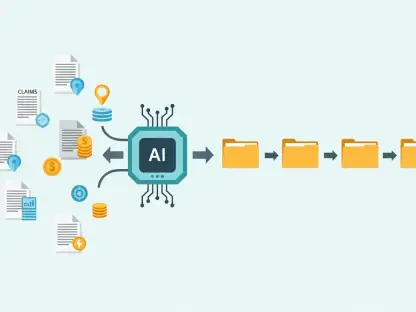
Medicare Summary Notices offer a comprehensive snapshot of the medical services and supplies received and billed. Every quarter, beneficiaries receive these statements for Part A and Part B services, while Medicare Advantage, Part D prescription plans, or Medigap plan holders receive similar documents known as Explanation of Benefits from their respective providers. These records outline several critical details, including services or supplies received, the amount paid by Medicare, what remains the beneficiary’s responsibility, and essential coverage notes. Understanding MSNs not only aids individuals in keeping track of their medical expenses but also equips them to identify discrepancies that may indicate fraudulent activity.
Having a clear understanding of one’s MSN is the first step toward identifying unauthorized charges. The first step in reviewing an MSN involves verifying basic information such as the beneficiary’s name, Medicare or account number, and the date of service. Next, it is crucial to review each listed service carefully, examining whether the recorded services were actually received on the noted dates and from the specified providers. This meticulous approach ensures accuracy and helps detect potential errors or fraudulent claims. Attention to detail when reviewing these notices is vital in maintaining financial transparency and preventing exploitation by unauthorized parties.
Detecting Discrepancies and Taking Action
When discrepancies arise within this system, swift action is imperative. One should never overlook suspicious charges, as they can point to fraudulent activities. These charges may include duplicate billings, unfamiliar services, or equipment not received, all of which serve as potential red flags. It is important to note the amounts that Medicare and the plan approved versus what was billed, and the portion the beneficiary is responsible for. This vigilance helps in promptly addressing errors before they escalate into more significant financial issues.
If a discrepancy is noted, contacting the health care provider to verify the billing should be the first step. Often, billing errors may occur, which can be corrected with simple communication. In instances where resolution is not attained with the provider, contacting Medicare directly via the 1-800-MEDICARE helpline is advisable to report suspected fraud. Additionally, beneficiaries can request a fraud alert to be placed on their account for further security. Local Senior Medicare Patrol offices also offer assistance, guiding beneficiaries through the process of reporting and resolving these discrepancies effectively.
The Broader Impact on Medicare Fraud
By reviewing MSNs diligently, beneficiaries contribute to safeguarding the entire Medicare system. Fraud and improper payments not only affect individuals but also challenge the sustainability of Medicare for future generations. Vigilant review of MSNs is not just a defensive measure for individual finances; it is a proactive stance that supports the longevity and efficiency of the Medicare program. With every careful review, beneficiaries play a crucial role in highlighting discrepancies and thwarting fraudulent attempts.
Encouraging a community-wide awareness and understanding of MSNs can have far-reaching effects on reducing fraud. Keeping a personal health journal to track appointments and acquired services, saving MSNs for at least a year, and utilizing digital resources like MyMedicare.gov to access electronic records, all contribute to a robust defensive strategy. During times such as Fraud Prevention Month and beyond, collective efforts can foster a secure environment for accessing essential medical benefits without fear of exploitation.
Moving Forward with Medicare Fraud Prevention
In today’s world, where scammers continually refine their deceptive strategies, Medicare beneficiaries have a crucial tool to help defend against health care fraud: the Medicare Summary Notice (MSN). This document meticulously lists the services and supplies billed to Medicare, effectively acting as a personal fraud detection mechanism. Health care fraud significantly impacts finances, siphoning billions from Medicare annually, which underscores the importance of comprehending and using the information provided in these notices. Vigilance in reviewing MSNs ensures that beneficiaries can spot discrepancies and errors in billing, thereby safeguarding themselves and preserving the integrity of the Medicare program. Being proactive in examining these statements also empowers beneficiaries to report any suspicious activity. By doing so, they contribute to a wider effort to combat fraud, ensuring that funds are used correctly, and maintaining trust in the system designed to support their well-being.