In today’s complex world of workers’ compensation, a critical yet often overlooked factor can dramatically shape the outcome of a claim, sometimes even more than the injury itself, and that factor is the social determinants of health (SDOH). These non-medical elements, such as income, housing stability, access to healthcare, and personal support systems, play a pivotal role in determining how swiftly and successfully an injured worker recovers. Imagine two employees with identical injuries: one returns to work within weeks, while the other lingers in recovery for months. What accounts for this disparity? The answer often lies in the social and environmental conditions surrounding each individual. As claim costs and complexities continue to escalate, understanding these societal influences becomes essential for employers, insurers, and claims managers. This article delves into the profound connection between SDOH and workers’ compensation, exploring why addressing these factors is not just a compassionate choice but a strategic necessity to control expenses and improve recovery timelines.
Unpacking the Role of Social Determinants in Recovery
Social determinants of health encompass the broader conditions in which individuals live, work, and age, significantly influencing their overall well-being beyond just medical care. In the realm of workers’ compensation, these factors include financial security, proximity to healthcare facilities, whether a worker resides in a rural or urban setting, and the strength of their personal support networks. Such elements often dictate a worker’s ability to attend medical appointments, adhere to prescribed treatments, or manage everyday tasks during recovery. When these determinants are unfavorable, they can transform a straightforward injury into a prolonged and costly claim. For instance, a lack of reliable transportation might prevent timely access to physical therapy, stalling progress. Recognizing SDOH as a key component of recovery allows stakeholders to address barriers that pure medical treatment cannot resolve, highlighting the need for a more comprehensive approach to claims management.
The impact of these social factors is not merely theoretical but manifests in tangible disparities in recovery outcomes. Consider a worker in a remote rural area who must travel long distances to see a specialist, often delaying critical interventions that could speed healing. Compare this to an urban worker with easy access to multiple clinics, where treatment begins almost immediately. Similarly, financial stress from lost wages can exacerbate mental health challenges, further slowing physical recovery. These examples underscore how social conditions create uneven playing fields, even for workers with identical injuries. Industry data supports this, showing that claims involving social barriers often result in longer disability durations and higher costs. Addressing SDOH, therefore, becomes a crucial step in leveling these disparities and ensuring that recovery is not derailed by circumstances outside a worker’s control.
Why Social Factors Drive Claim Complexity
The influence of social determinants on workers’ compensation claims extends far beyond individual recovery, contributing to systemic challenges within the industry. Research indicates that non-medical issues, such as mental health struggles tied to financial instability or chronic conditions worsened by poor living environments, often lead to extended periods of temporary disability and ballooning medical expenses. A worker grappling with anxiety over unpaid bills may experience slower physical healing due to stress, while another without nearby healthcare options might miss vital treatments, allowing minor injuries to worsen. These social factors don’t just affect the injured individual; they ripple outward, increasing litigation risks and creating unpredictability for insurers and employers. Tackling these underlying issues is essential to prevent small setbacks from evolving into major, costly obstacles that strain the entire claims process.
Moreover, the broader implications of ignoring social determinants can destabilize the workers’ compensation system as a whole. As claim severity rises, driven by these unaddressed barriers, organizations face mounting pressures from both financial and regulatory standpoints. The connection between social conditions and claim outcomes reveals a critical gap in traditional approaches that focus solely on medical treatment. Experts emphasize that understanding and mitigating these factors can significantly reduce the frequency of prolonged claims and associated disputes. By shifting focus to include the social context of an injury, stakeholders can better predict potential complications and allocate resources more effectively. This perspective reframes SDOH not as peripheral concerns but as central drivers of claim complexity, urging a more integrated strategy to manage costs and improve worker well-being across the board.
Strategies for Early Intervention to Mitigate Social Barriers
One of the most promising ways to counteract the effects of social determinants on workers’ compensation claims is through early intervention. The initial weeks following an injury represent a critical period to identify and address barriers such as lack of transportation, inadequate support systems, or financial pressures that could hinder recovery. Training intake staff, particularly nurses, to collect detailed information about a worker’s psychosocial and environmental circumstances during the first assessment can uncover risks that might otherwise go unnoticed. For example, discovering that a worker lacks reliable childcare during recovery allows for tailored solutions before the issue delays treatment adherence. This proactive stance enables claims managers to customize recovery plans to fit the unique needs of each individual, ensuring that social obstacles are tackled head-on rather than allowed to fester into larger problems.
Beyond identifying risks, early intervention relies on structured protocols and active engagement with all parties involved in a claim. High-touch communication between workers, healthcare providers, and employers during the first month post-injury helps establish clear, evidence-based treatment plans and return-to-work timelines. Documenting social factors within claims management systems allows adjusters to prioritize resources for high-risk cases, preventing minor delays from escalating into significant setbacks. This approach not only enhances recovery outcomes for the injured worker but also minimizes the likelihood of costly disputes or extended disability periods. By embedding early detection and personalized support into the claims process, the industry can address social determinants in a way that benefits both the individual and the broader system, reducing financial strain and fostering quicker resolutions.
Leveraging Technology to Address Social Influences
Technology is rapidly transforming how the workers’ compensation industry manages the impact of social determinants on claims, offering tools that enhance precision and efficiency. Advanced claims platforms now employ predictive analytics to evaluate a range of data points, including a worker’s geographic location, medical history, and potential social risks. These systems generate real-time alerts for adjusters, flagging cases that may require additional support due to barriers like limited healthcare access or financial instability. For instance, a platform might highlight a worker in a rural area as high-risk for delayed treatment due to travel constraints, prompting immediate action. Such technological innovations enable stakeholders to intervene before small issues grow into expensive complications, streamlining the claims process while ensuring that social factors are not overlooked in recovery planning.
However, while technology offers powerful solutions, it must be paired with human expertise to achieve the best results in addressing social determinants. Predictive models and automated alerts provide valuable insights, but they cannot fully capture the nuances of a worker’s situation without the judgment of experienced adjusters and case managers. Building rapport with injured workers and interpreting data in the context of individual circumstances remain indispensable components of effective claims management. The combination of data-driven tools and personal interaction creates a balanced approach, ensuring that interventions are both timely and empathetic. As technology continues to evolve, its role in integrating social factors into claims strategies will likely expand, offering even greater potential to improve outcomes while maintaining the human touch that underpins successful recovery support.
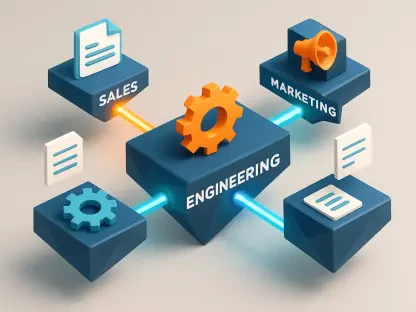
Future Steps for a Holistic Claims Approach
Reflecting on the challenges posed by social determinants in workers’ compensation, it has become evident that past approaches often fell short by focusing narrowly on medical treatment. Efforts to manage claims in previous years revealed how non-medical barriers, such as inadequate housing or limited access to care, consistently prolonged recovery and inflated costs. The industry grappled with rising claim complexities, driven by factors that traditional systems were not equipped to address. Historical data showed that workers facing social challenges frequently encountered extended disability durations, underscoring the need for a shift in perspective. These past struggles highlighted the urgency of integrating social considerations into claims management, paving the way for more innovative and inclusive strategies that have emerged over time.
Looking ahead, the path forward involves adopting a more holistic approach that prioritizes both early action and technological integration to tackle social determinants effectively. Stakeholders should invest in training programs for claims staff to better recognize and address non-medical barriers from the outset. Additionally, expanding the use of predictive analytics and exploring emerging tools like artificial intelligence can refine the ability to anticipate risks tied to social factors. Collaboration among employers, insurers, and healthcare providers will also be key to creating supportive environments that facilitate recovery. By committing to these actionable steps, the industry can build a framework that not only mitigates the impact of social determinants but also fosters sustainable improvements in worker outcomes and cost management for the long term.