In a significant pivot that reflects the mounting economic pressures on businesses across the United States, employers are now placing a higher premium on controlling employee benefit costs than on using those same benefits as a tool for attracting and retaining top talent. An annual analysis of 1,241 employers reveals a stark reversal from the previous year, with fiscal management now taking precedence. This strategic realignment is not a simple cost-cutting measure but a sophisticated response to the relentless rise of medical and pharmacy expenses. Companies are navigating a complex landscape, striving to rein in expenditures without undermining the competitive benefits packages essential for maintaining a skilled workforce. The central challenge lies in implementing effective cost-containment strategies that do not simply transfer the financial burden to employees, a move that could prove counterproductive in a tight labor market. This shift signals a new era of fiscal discipline in benefits management, demanding innovative solutions and a re-evaluation of long-held strategies to balance financial health with human capital needs.
The New Financial Tightrope
Beyond Shifting the Burden
In response to escalating healthcare inflation, organizations are deploying a host of sophisticated cost-management tactics designed to enhance efficiency and control spending from within the system, rather than resorting to the straightforward but often demoralizing practice of increasing employee contributions. A primary area of focus involves a detailed re-evaluation of stop-loss plan structures, which protect companies from catastrophic claims. By adjusting attachment points and coverage terms, employers can better manage their risk exposure and predictable costs. Simultaneously, there is a growing emphasis on stricter audit practices for claims and administrative services, ensuring that payments are accurate and that plan partners are held accountable for their performance. Furthermore, companies are increasingly forming strategic partnerships with digital health providers. These collaborations are aimed at improving care navigation, promoting preventive health measures, and providing greater transparency into treatment costs and outcomes, thereby empowering both the employer and the employee to make more informed and cost-effective healthcare decisions.
This strategic pivot towards internal optimization reflects a deeper understanding that sustainable benefits programs require more than just annual budget adjustments. The goal is to build a more resilient and efficient healthcare delivery model that can withstand future economic shocks and inflationary pressures. By focusing on the structural components of their health plans, employers are engaging in a form of financial stewardship that seeks to preserve the long-term value of their benefits offerings. This approach acknowledges that employee benefits are a critical investment in human capital, and eroding that investment through direct cost-shifting can have significant negative impacts on morale, productivity, and retention. Therefore, the implementation of these nuanced strategies is not merely a defensive reaction to rising costs but a proactive effort to fortify the company’s competitive position by ensuring that its benefits remain both attractive to talent and financially viable for the organization over the long haul.
Refining Coverage to Retain Talent
Interestingly, the intense focus on cost containment has not led to a widespread reduction in the quality of benefits. On the contrary, data from consulting firms reveals a concurrent trend of strategic benefit enhancements aimed directly at supporting talent acquisition and retention. A notable 31% of employers have recently improved their medical benefits, while 12% have upgraded their pharmacy offerings. This seemingly contradictory behavior highlights the delicate balance that companies are striving to achieve. They recognize that in a competitive labor market, a robust benefits package remains a powerful differentiator. Consequently, rather than making across-the-board cuts, organizations are selectively investing in areas of coverage that provide the most significant value and appeal to current and prospective employees. This targeted approach allows them to address specific workforce needs and market demands without derailing their broader cost-management objectives, demonstrating a nuanced understanding of benefits as a strategic tool rather than just an operational expense.
The refinement of coverage is a data-driven process, where employers analyze utilization patterns, employee feedback, and market benchmarks to identify opportunities for high-impact improvements. For instance, an enhancement might involve expanding mental health support, introducing more comprehensive virtual care options, or lowering out-of-pocket costs for high-value services that have been proven to improve health outcomes and reduce long-term expenses. This surgical approach to benefit design ensures that every dollar invested is maximized for its effect on both employee well-being and the company’s ability to compete for talent. It signals a move away from a one-size-fits-all model towards a more personalized and strategic framework. By carefully curating their benefits portfolio, employers can send a clear message that they are committed to supporting their workforce, even as they navigate a challenging economic environment, thereby fostering loyalty and reinforcing their status as an employer of choice.
A Continued Investment in the Workforce
Prioritizing Wellbeing and Family Support
Despite the overriding pressure to manage expenses, corporate investment in workforce support and overall well-being has remained remarkably resilient. An impressive 77% of employers now integrate comprehensive wellbeing programs directly into their healthcare strategies, viewing them not as a peripheral perk but as a core component of a healthy and productive workforce. This commitment is further underscored by the fact that among these companies, a significant 78% are planning to increase their budgets for these initiatives in the near future. This sustained investment indicates a broad recognition that employee well-being is intrinsically linked to organizational performance. Proactive support for physical, mental, and financial health can lead to reduced absenteeism, lower long-term healthcare costs, and higher employee engagement, making it a sound strategic investment rather than a discretionary expense, even in times of fiscal constraint.
This dedication to employee support extends deeply into family-oriented benefits, which continue to be a key priority for a majority of organizations. The data reveals that 71% of employers now offer paid parental leave policies that surpass the minimums mandated by state or federal law. This widespread commitment signals a clear understanding of the evolving needs of the modern workforce, where support for caregivers is a critical factor in attracting and retaining skilled professionals. By providing generous leave policies, companies are not only supporting the health and well-being of new parents but are also fostering a more inclusive and loyal company culture. This continued focus on family-centric benefits, even amidst tightened budgets, illustrates that employers are making deliberate choices to invest in policies that have a profound and lasting impact on their employees’ lives and, by extension, on the long-term success of the business.
The Case of GLP-1 Medications
The complex challenge of covering GLP-1 drugs for weight loss serves as a powerful microcosm of the dual strategy employers are now employing. Nearly half of all surveyed employers (48%) currently cover these highly effective but expensive medications, demonstrating a willingness to provide access to cutting-edge treatments that can significantly improve employee health. Moreover, of those that offer coverage, an overwhelming 89% plan to continue doing so for the next one to two years. This strong commitment shows that employers are not shying away from shouldering the substantial cost of innovative pharmaceuticals when the potential benefits to employee health and productivity are clear. They are embracing advancements in medical science as part of their overall benefits philosophy, recognizing that addressing conditions like obesity can have a positive downstream impact on a host of related health issues, ultimately contributing to a healthier and more resilient workforce.
However, this access is almost universally paired with rigorous cost-control measures to manage the significant financial impact of these drugs. The provision of GLP-1s is not an open-ended entitlement but a carefully managed benefit. Over 63% of employers that cover these medications have implemented significant restrictions to control utilization and costs. Nearly half of those have instituted clinical requirements that are even stricter than the standard guidelines set by the U.S. Food and Drug Administration. These limitations may include higher body mass index (BMI) thresholds, mandatory participation in lifestyle modification programs, or prior authorization processes that require extensive documentation of medical necessity. This layered approach perfectly exemplifies the broader trend: employers are willing to invest in valuable, high-cost treatments but are simultaneously implementing sophisticated guardrails to ensure that the benefit is used appropriately and that its financial impact remains sustainable for the organization.
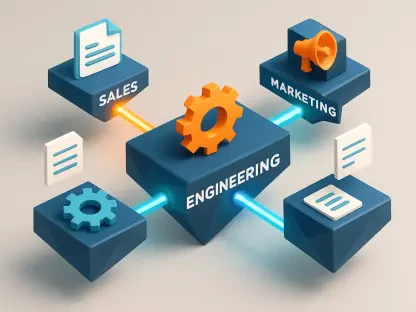
A Look at the Strategic Realignment
Ultimately, the recent shift in employer priorities reflected a sophisticated strategic realignment rather than a simple retreat from workforce investment. Faced with undeniable fiscal pressures from healthcare inflation, organizations did not abandon their commitment to providing competitive benefits. Instead, they adopted a more disciplined and multifaceted approach to benefits management. This involved implementing robust internal cost-control mechanisms, such as stricter audits and innovative digital health partnerships, which sought efficiency from within the system. Concurrently, they made targeted enhancements to medical and family-support benefits to maintain their competitive edge in the labor market. The careful management of high-cost treatments like GLP-1 drugs encapsulated this dual strategy, where access was provided but governed by strict financial and clinical controls. This period was characterized by a move toward greater financial stewardship, ensuring the long-term sustainability of the very benefits that remained crucial for attracting and retaining the talent needed to drive future growth.